PERFACT Procedure by Dr Pankaj Garg
PERFACT PROCEDURE: A new concept to treat highly complex anal fistulas
(PERFACT- Proximal superficial cauterization, emptying regularly of fistula tracts and curettage of tracts)
BRIEF About The Procedure
Perfact procedure is a simple, economical and novel method to cure complex fistula-in-ano. It is associated with minimal pain and morbidity and least risk of incontinence as both the anal sphincters are completely preserved. It is quite effective in complex fistula cases where other methods do not have high success rate like horseshoe fistula, fistula with multiple tracts, recurrent fistula and fistula with supralevator extension. Perfact procedure is also quite successful in cases where internal opening cannot be localized. In patients presenting with perianal/ischiorectal abscess, it can be done as a definitive first line procedure on initial presentation (instead of two stage operations where incision and drainage is done as the initial intervention and definitive fistula surgery is done later). Perfact procedure is not indicated for low simple anal fistulas.
Indications
All types of complex fistula-in-ano
- Fistula associated with multiple tracts
- Horse shoe fistulas
- Recurrent fistulas
- Anterior fistula in females
- Fistula with long tracts (any tract length > 10 cms)
- Fistula with supralevator blind extension (not with high rectal opening)
- Fistula where internal opening cannot be localized
- Fistula associated with abscess/ pus collections. It was used as a first line definitive procedure in patients of anal fistulas presenting with ischiorectal or perianal abscess.
Contraindications
- Simple low fistula
- Fistula with supralevator rectal opening (on MRI and/or examination on operating table)
Method
Perfact procedure had three steps (Figure- 1)
1. Proximal superficial cauterization- The area around the internal opening was freshened and de-epithelized by electrocautery and the wound was encouraged to heal by secondary intention (granulation tissue). This usually closed the internal opening in about 10-12 days.
2. Curettage of tracts- All the tracts were thoroughly curetted and debrided of their lining with a curette.
3. Emptying regularly of fistula tracts- The curetted tracts were kept clean and empty of any serous fluid so as to ensure that the tracts healed (close) by granulation tissue. Keeping all the tracts clean till they healed completely was a challenging task and the most demanding step of the procedure. It took 4 to 8 weeks (occasionally even longer) for all the tracts to heal fully. Till that time, regular cleaning of the tracts was done.
To ensure proper cleaning of the tracts, the following steps (one or multiple depending upon the requirement and fistula characteristics) could be done in a patient
A. Multiple holes were made along the straight or the horseshoe tract in such a way that the farthest corner of the tract could be cleaned with ease.
B. The external opening was widened and the scarred puckered skin (if present) was excised. The aim was to make the opening bigger than 1 x 1 cms. This facilitated cleaning of the tracts for a longer duration.
C. Loose rubber setons were inserted in the holes to prevent their premature closure. These were removed 10-12 days after the operation.
Intra-operative
A saddle block (spinal anesthesia) or a short general anesthesia was given. The patient was positioned in a lithotomy or a prone jack-knife position. The internal opening was localized. This was facilitated by injecting saline, povidine iodine or hydrogen peroxide through the external opening.
Proximal superficial cauterization was carried out with electrocautery around the internal opening, cauterizing only the mucosa and superficial part of the internal sphincter. The crypt glands, the internal opening and the tissue around it were cauterized. This usually resulted in an oval area, approximately 1 cm (wide) and 2 cm (long), with internal opening at the centre of the wound. After cauterization, the wound was left as such and no attempt was made to close the internal opening with any suture, stapler, glue or plug.
After this, the tracts were curetted in accordance with the MRI diagram and the tract lining was scrapped out as much as possible with a blunt curette. While doing so, a finger was kept in the rectum so as to ensure that the curette didn’t accidentally perforate the rectum.
The patient was discharged on the operation day (if done under short general anesthesia) or the first postoperative day (if done under saddle or spinal anesthesia). He/she could resume all his/her normal activities on the same day. The patient was encouraged to walk briskly for 5 kilometers every day. This helped in keeping the tracts empty.
Postoperative cleaning aimed at healing of two areas – the cauterized wound in the anal canal (around the internal opening) and the curetted tracts. The former was pivotal as the closure of the internal opening depended upon it and generally took about 10-12 days to heal. The latter was also needed for the complete closure of the fistula and took a variable time (4-8 weeks) depending on the fistula characteristics (number, length and complexity of the tracts) and the patient co-morbidities (diabetes, anemia, hypoproteinemia etc).
The cleaning process entailed cleaning the cauterized wound in the anal canal and regular cleaning and emptying of the curetted tracts. The former was done by gentle rubbing of the wound by doing a per rectal finger insertion. The latter was done by a cotton swab mounted on an artery forceps. No povidine iodine, hydrogen peroxide or any liquid was injected in the tract during the cleaning process as this would have prevented the internal opening from closing. The cleaning was done by a trained nurse, a medical attendant or a relative. In our setting, teaching a relative was an economical and a preferred option.
The cleaning process was done four times a day. For the first 10 days, the patient was called to the outpatient clinic for supervised cleaning once or twice a day depending upon the complexity of the fistula. After this, the patient could do the cleaning process at home.
Result
We have done 102 patients in the last two years. The median follow-up was 16 months (5-24 months). The mean age was 42.7 ± 11.3 years. Males/Female ratio was 86/16. Fistula was recurrent in 76.5% (78/102), horseshoe in 50.1% (52/102), had multiple tracts in 52.9% (54/102), had associated abscess in 41.2% (42/102), was anterior in 33.3% (34/102), internal opening not found in 15.7%(16/102) and had supralevator extension in 9.8% (10/102). Fourteen patients were excluded (lost to follow up ). The success rate was 86.4% (76/88) and the recurrence rate was 13.6% (12/88). There was no significant change in objective incontinence scores three months after the operation. The pain was minimal with all patients resuming their normal activities with in 72 hours of operation.
Conclusion
Perfact procedure is a new effective method for complex fistula-in-ano, effective even in fistulas with supralevator extension, internal opening not localizable and fistula associated with abscess.
Figure-1: PERFACT Procedure- an overview
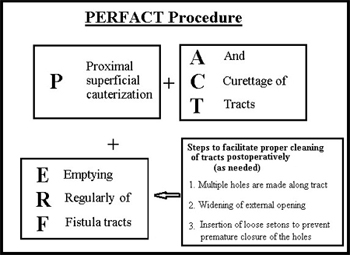
Figure-2: Preoperative MRI of Perianal region & its Schematic diagram showing a recureent horseshoe abscess & fistula from 2 to 10 o’clock position in a 29 yr old female patient. There was no external opening and the internal opening was at posterior midline.
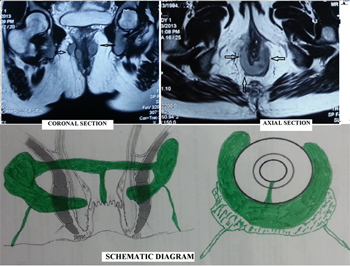
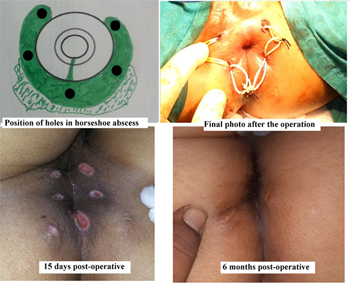
Figure-3: Management of a 29 yr old female patient by Perfact procedure having a horseshoe abscess and fistula from 2 to 10 o’clock. There was no external opening and the internal opening was at posterior midline. The right bottom picture shows complete healing of the fistula (MRI & diagram of this patient shown in Figure 2)
Dr Pankaj Garg
Colorectal Surgeon
Garg Clinics,
1042, Sector-15
Panchkua, Hayan
Email: [email protected]
M-9501011000
This procedure has been presented as
- Podium Presentation at ASCRS (American Society of Colon Rectum Surgeons) annual meeting at Fort Lauderdale, Florida, USA on 21 May 2014
- Poster Presentation at Tripartite Colorectal Meeting 2014 at Edinburgh, UK on 1 July 2014.
- Podium Presentation at ASI (Association of Surgeons of India) annual conference at Ahmedabad, India on 28th December 2013
- Podium Presentation at ACRSI (Association of Colon Rectal Surgeons of India) annual conference at Khajuraho, India on 22th September 2013
Accepted for publication in World Journal of Gastroenterology
